Food, Global Health Reading time 3 min
Tuberculosis: a new lead for biomarkers to assess the risk of transmission
Published on 21 May 2024
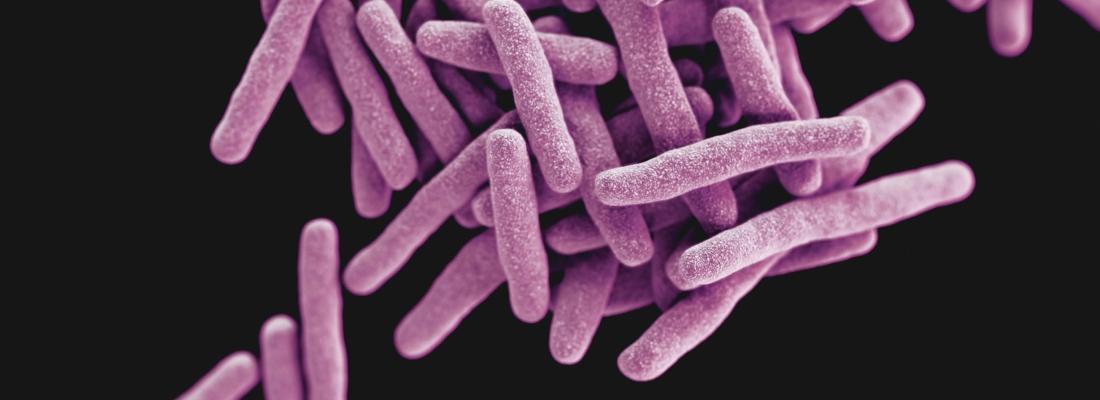
Tuberculosis is a chronic inflammatory disease which most often targets the lungs. It is caused by Mycobacterium tuberculosis and has afflicted humans for thousands of years. Far from a thing of the past, the disease remains all too active throughout the world and killed 1.3 million people[1] in 2022. Monitoring the development of tuberculosis is difficult, and tests do not distinguish between the active (contagious) and latent (non-contagious) forms of the disease. It is estimated that one-third of the world’s population is infected with the latent – and most common – form of TB, which presents no clinical symptoms. Detecting which individuals are likely to transmit the bacteria to others is therefore of imminent importance.
A team of scientists from INRAE and Inserm, with researchers in Brazil and Belgium, have studied neutrophils, a type of white blood cell armed with a toxic arsenal to kill pathogens. A massive concentration of these cells in infected areas, however, can destroy tissue – most often lung tissue in cases of tuberculosis.
The research team discovered two subsets of neutrophils that play opposing roles in the inflammation process triggered by an M. tuberculosis infection: conventional neutrophils, which exacerbate inflammation by producing IL-1β, a pro-inflammatory cytokine, and regulatory neutrophils, which “brake” inflammation using PD-L1 protein to suppress pro-inflammatory T-cell proliferation. This neutrophil subset tempers immune response and prevents lung damage. Researchers demonstrated that injecting regulatory neutrophils into mice that are highly vulnerable to M. tuberculosis minimised lung tissue lesions. These findings bring to light the risks of prescribing anti-PD-L1 in certain cancer treatments for patients with latent tuberculosis. This type of treatment, sometimes used to reverse the inactivation of an immune system caused by cancer cells, could also reactivate a TB infection by blocking the action of PD-L1.
The scientists also showed that the most virulent strains of the bacteria were able to counteract regulatory neutrophil activity and create a self-benefiting inflammatory environment by inhibiting the production of PD-L1.
These findings represent a step forward in the diagnosis of a patient’s clinical condition, from latent and asymptomatic to active infection, based on concentrations of conventional and regulatory neutrophils in the blood. The detection of neutrophil subsets as biomarkers would make it possible to tailor the prescription of antibiotics to individuals at risk of developing a contagious form of TB. The feasibility of this detection will be further explored by researchers in collaboration with clinicians.
[1] Based on the World Health Organization (WHO) Global Tuberculosis Report 2023
tuberculosIS WORLDWIDE IN 2022 (2023 WHO report)
- The reported number of people newly diagnosed with TB was 7.5 million in 2022 (the highest number since WHO began global TB monitoring in 1995).
- COVID-19 related disruptions caused nearly half a million additional deaths from tuberculosis between 2020 and 2022.
- Two-thirds of all cases were in eight countries: India (27%), Indonesia (10%), China (7.1%), the Philippines (7.0%), Pakistan (5.7%), Nigeria (4.5%), Bangladesh (3.6%) and the Democratic Republic of Congo (3.0%).
- 34 million people received treatment.
- Treatment success rates have improved: to 88% for people treated for drug-sensitive TB and 63% for people with multidrug-resistant or rifampicin-resistant TB (MDR/RR-TB).
REFErence
Doz-Deblauwe E., Bounab B., Carreras F. et al. (2024). Dual neutrophil subsets exacerbate or suppress inflammation in tuberculosis via IL-1β or PD-L1. Life Science Alliance, DOI: 10.26508/lsa.202402623
