Food, Global Health Reading time 2 min
Discovery of a mechanism that allows Staphylococcus aureus to survive in blood
Published on 06 May 2024
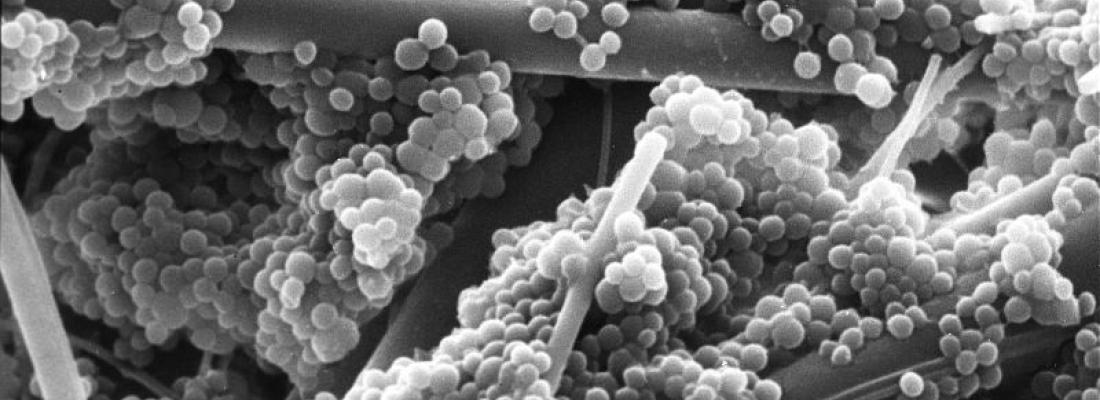
Bacterial infections are the second leading cause of death in the world and golden staph, Staphylococcus aureus, is among the deadliest. In 2019, golden staph was deemed to have caused more than one million deaths worldwide and more than 16,000 in France, according to a study published in 2022 in The Lancet. In France, it is one of the main pathogens behind nosocomial (hospital) infections and food poisoning. At the current time, antibiotics are the only effective treatment, but resistant strains have emerged, which leads to the risk of a therapeutic impasse[1]. This is why an INRAE research team, in collaboration with the CEA and CNRS, have been studying Staphylococcus aureus for several years now, in particular to find out how it survives in blood.
Blood: a hostile environment for bacteria
Mammal blood contains red blood cells, which are responsible for transporting oxygen. Those cells contain a large amount of a molecule called heme, which is notably used to bind oxygen. But heme is toxic to bacteria or other cells when it is located outside red blood cells. When pathogenic bacteria like Staphylococcus aureus are in the bloodstream, they cause hemolysis, i.e. the red blood cells burst and free up heme. They can then come into contact with the heme, which is toxic to them.
These researchers discovered that Staphylococcus aureus can detect heme using a specific sensor named HssS, which is found on its membrane. When the sensor detects heme, it triggers a defense mechanism in golden staph, which synthesizes a heme efflux pump that ejects that substance from the bacterium. This creates a protective barrier that allows Staphylococcus aureus to survive in the bloodstream and spread the infection. Laboratory trials have shown that the virulence of those golden staph strains that do not have the HssS sensor and so, are incapable of detecting heme is much weaker.
A way forward for new and innovative antibiotic strategies
Given the problems with antibiotic resistance, these results open new pathways for antibiotic strategies to control Staphylococcus aureus by identifying molecules that inhibit the HssS sensor, thereby decreasing the bacterium's virulence. In addition, since the HssS sensor is specific to pathogenic bacteria, antibiotic strategies that target it will be more focused and, in theory, will not affect bacteria that are beneficial for our bodies, such as those that make up the intestinal microbiota.
Reference
Saillant V. et al. HssS activation by membrane heme defines a paradigm for 2-component system signaling in Staphylococcus aureus. mBio, 29 April 2024, DOI: https://doi.org/10.1128/mbio.00230-24
