Food, Global Health Reading time 2 min
Microbiota, the intestinal revolution - Feed your microbiota
Published on 30 November 2017

Fibre: what drives microbiota
Fibre, those long chains of polysaccharides that abound in fresh or dried vegetables, fruits and cereals, is what makes the microbiota thrive. Our commensal bacteria form a sort of assembly line in reverse, breaking down and fermenting fibres, each species with its specific enzymes in its rightful spot along the line, playing a specific role. The bacteria break fibre down into smaller and smaller units. When a diet is poor in fibre, it is this process and this bacterial diversity that suffer. INRA researchers have shown that the greater the intake of fibre, the greater the diversity and number of bacterial species, and the more stable and balanced our microbiota. And that is not all: the breakdown of fibre produces short-chain fatty acids (SCFAs) that are known to protect health. For starters, they regulate inflammatory processes and stimulate the production of glucose in the intestines, which makes us feel full and curbs food intake. SCFAs are also known to staunch the proliferation of cancer cells in the colon. Need another reason to be nice to your microbiota?
What happens to dietary fibre?
Until now, it was thought that the breakdown of dietary fibre (and especially complex polysaccharides) took place only in the colon. Now we know that this is a major function of intestinal microbiota. Thanks to metagenomic approaches, INRA researchers working with the CNRS have revealed the presence of fibrolytic activity in the small intestine, and more specifically in the ileum. These findings are causing science to rethink how dietary fibre is processed and what impact it has on human health.
Modaltub and the fate of an apple
What happens when you bite into an apple? This simple act triggers the extremely sophisticated process of breaking down food. From chewing to fermentation in the intestines, the components of food - its fibre, proteins and cell walls - are broken down so that nutrients can be sent into the blood stream and waste evacuated. INRA’s Modaltub project aims to study how this process works with the help of artificial digesters and mathematical models that simulate what happens in each part of the digestive system. The scientists have already succeeded in imitating the mouth, stomach and small intestines. Next up: the colon and creating an artificial microbiota. The goal is to mime digestion by adjusting various key parameters such as pH and redox potential*. The scientists will also be able to study how food is processed and assimilated depending on their initial structure. Ultimately, the data gathered will be used to create digital simulations of the digestive process.
Obesity: are microbes to blame?What constitutes a “good” intestinal microbiota? From an evolutionary point of view, it is one that makes the most of the energy that food provides. But when the energy balance is upset due to a diet too high in sugar and fat, the microbiota can no longer regulate energy flow. A microbiota thus disturbed now participates in maintaining this imbalance, and the body responds by storing too much fat in its adipose tissue. Scientists have studied the microbiota of obese people in comparison to that of healthy subjects, and found significant differences: the diversity and richness of intestinal bacteria is most compromised in obese people, and their microbiota can no longer safeguard health. Although they cannot be said to be solely responsible for obesity, some bacterial species very probably play a prominent role in weight gain and the inflammatory processes associated with it. Scientists hope to characterise those bacteria, analyse their genome, and gain a better understanding of their functions in order to combat this epidemic. |
Unhappy intestines refuse to be ignored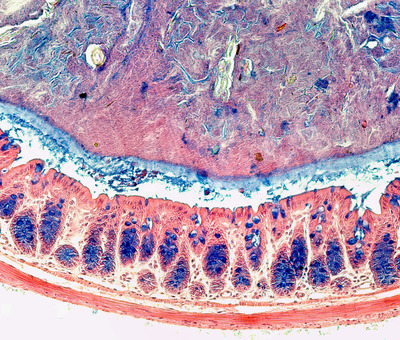
Stomach aches? Constipation? Diarrhoea? Some 10 to 20% of French people suffer from irritable bowel syndrome (IBS), a disorder with multiple causes as yet poorly understood and capable of making daily life miserable. To better understand this syndrome, researchers are turning to the microbiota. An INRA team has showed that IBS patients illustrate serious imbalances in intestinal microbiota. The result is that for one and the same food, a person with IBS produces less butyrate, a fatty acid that has protective properties, and more hydrogen and sulphides that may be at the root of abdominal pain. These findings have led to a new avenue for treatment: it all comes down to one type of bacteria present in the intestine that is capable of reducing the production of gas and sulphides. Experiments carried out on mice and humans have shown that administering these bacteria allows the body to redress metabolic flows and reduce symptoms. |
What to do with so much protein?Modern societies are very fond of protein: on average, the French consume 1.7 times more than recommended quantities. However, some people, like athletes seeking to boost their performance, or the elderly who struggle to fight dwindling muscle mass, need more protein than others. Furthermore, high-protein diets designed to help people trim down are all the rage, despite repeated risk warnings. The question remains, how does this over-consumption of protein affect the intestines? INRA researchers set out to find the answer and learned that a portion of surplus protein is neither digested nor assimilated by the body. When surplus protein passes through the colon, it is broken down by bacteria in the microbiota. This process generates molecules (such as hydrogen sulphide p-cresol) that are toxic for the cells of the intestinal mucosa, and can even alter their DNA. When they pass into the bloodstream, they can also have a negative impact on some organs such as the kidneys. Scientists hope to use these findings to fine-tune dietary recommendations in certain populations in order to ensure that the benefits of a high-protein diet outweigh the risks. |
